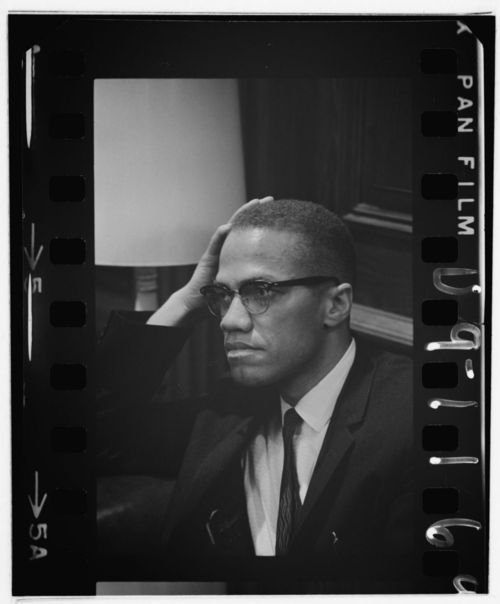
suave smooth cool hint of geek Gregory Peck in to kill a mocking bird try the same look get designer glasses online 2for1 on all glasses including lens and coating with free post to anywhere in europe from £50 http://www.freshoptical.co.uk/50-glasses.html
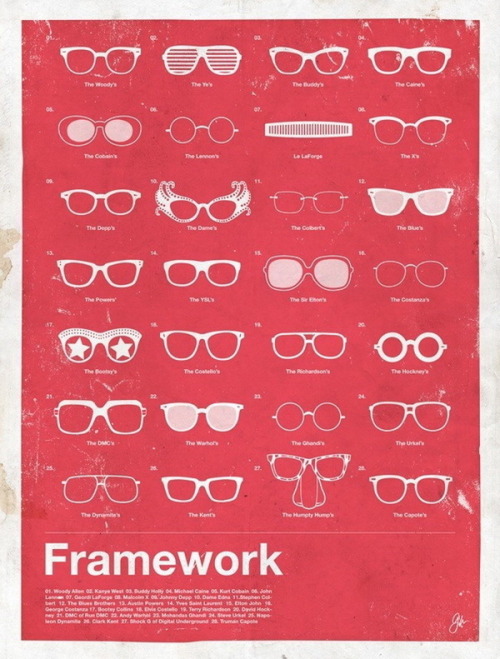
a guide to eyes eye tests spectacles and the best looking and stylish glasses wearers ever to walk the face of the planet oh and some funnies
Sunday 31 July 2011
Mick Jagger godlike staus ,The Stones
Mick Jagger god what a legend. For me the Stones were so much more edgy than the Beatles with better music.
glasses online 241 glasses from £50 free post
Glaucoma the facts
Diagnosis
Visual Field Test
Visual field is an important measure of the extent of damage to your optic nerve from elevated IOP. In glaucoma, it is the peripheral (side) vision that is most commonly affected first. Testing your visual field lets your doctor know if peripheral vision is being lost. There are several methods of examination available to your doctor; visual field testing has advanced significantly in recent years.
Ophthalmoscopy
Using an instrument called an ophthalmoscope, your eye doctor can look directly through the pupil at the optic nerve. Its color and appearance can indicate whether or not damage from glaucoma is present and how extensive it is. This technique remains the most important in diagnosing and monitoring glaucoma.
Normal-tension glaucoma is thought to be related, at least in part, to poor blood flow to the optic nerve, which leads to death of the cells which carry impulses from the retina to the brain. In addition, these eyes appear to be susceptible to pressure-related damage even in the high normal range, and therefore a pressure lower than normal is often necessary to prevent further visual loss.
Research in the field of optic nerve blood flow and its role in glaucoma is a source of much excitement at the present time and, hopefully, will lead to new methods of treating this disorder. Since the best therapy for normal-tension glaucoma is largely unknown, much attention is being given to a study known as the International Collaborative Low Tension Glaucoma Protocol.
Myopic (nearsighted) eyes have a concave-shaped iris which creates an unusually wide angle. This causes the pigment layer of the eye to rub on the lens. This rubbing action causes the iris pigment to shed into the aqueous humor and onto neighboring structures, such as the trabecular meshwork. Pigment may plug the pores of the trabecular meshwork, causing it to clog, and thereby increasing the IOP.
Miotic therapy is the treatment of choice, but these drugs in drop form can cause disabling visual blurring in younger patients.
Fortunately, a slow-release form is available. Laser iridotomy is presently being investigated in the treatment of this disorder.
Exfoliation syndrome can lead to both open-angle glaucoma and angle-closure glaucoma, often producing both kinds of glaucoma in the same individual. Not all persons with exfoliation syndrome develop glaucoma. However, if you have exfoliation syndrome, your chances of developing glaucoma are about six times as high as if you don´t. It often appears in one eye long before the other, for unknown reasons. If you have glaucoma in one eye only, this is the most likely cause. It can be detected before the glaucoma develops, so that you can be more carefully observed and minimize your chances of vision loss.
Ten percent of primary congenital glaucomas are present at birth, and 80 percent are diagnosed during the first year of life. The pediatrician or family first notice eye signs of glaucoma including clouding and/or enlargement of the cornea. The elevated intraocular pressure (IOP) can cause the eyeball itself to enlarge and injury to the cornea. Important early symptoms of glaucoma in infants and children are poor vision, light sensitivity, tearing, and blinking.
Pediatric glaucoma is treated differently than adult glaucoma. Most patients require surgery and this is typically performed early. The aim of pediatric glaucoma surgery is to reduce IOP either by increasing the outflow of fluid from the eye or decrease the production of fluid within the eye. One operation for pediatric glaucoma is goniotomy. Its rate of success is associated with the age of the child at the time of diagnosis, the type and severity of the glaucoma, and the surgery technique. Other surgical options are trabeculectomy and glaucoma drainage tubes.
Your Optician has a variety of diagnostic tools which aid in determining whether or not you have glaucoma -- even before you have any symptoms. Let us explore these tools and what they do.
The Tonometer
The tonometer measures the pressure in your eye. Your doctor places a numbing eye drop in your eye. Then you sit at a slit-lamp, resting your chin and forehead on a support that keeps your head steady. The lamp, which lets your doctor see a magnified view of your eye, is moved forward until the tonometer, a plastic prism, barely touches the cornea to measure your IOP. The test is quick, easy and painless.
The Tonometer
The tonometer measures the pressure in your eye. Your doctor places a numbing eye drop in your eye. Then you sit at a slit-lamp, resting your chin and forehead on a support that keeps your head steady. The lamp, which lets your doctor see a magnified view of your eye, is moved forward until the tonometer, a plastic prism, barely touches the cornea to measure your IOP. The test is quick, easy and painless.
The Pachymeter
The pachymeter measures central corneal thickness (CCT). Like the tonometer, your doctor will first anesthetize your eyes. Then a small probe will be placed perpendicular to the central cornea.
The pachymeter measures central corneal thickness (CCT). Like the tonometer, your doctor will first anesthetize your eyes. Then a small probe will be placed perpendicular to the central cornea.
CCT is an important measure and helps your doctor interpret your IOP levels. Some people with thin central corneal thickness will have pressures that are actually higher than when measured by tonometry. Likewise, those with thick CCT will have a true IOP that is lower than that measured. Measuring your central corneal thickness is also important since recent studies have found that thin CCT is a strong predictor of developing glaucoma in patients with high IOP.
Visual Field Test
Visual field is an important measure of the extent of damage to your optic nerve from elevated IOP. In glaucoma, it is the peripheral (side) vision that is most commonly affected first. Testing your visual field lets your doctor know if peripheral vision is being lost. There are several methods of examination available to your doctor; visual field testing has advanced significantly in recent years.
In computerized visual field testing you will be asked to place your chin on a stand which appears before a concave computerized screen. Whenever you see a flash of light appear, you press a buzzer. At the end of this test, your doctor will receive a printout of your field of vision. New software has been developed to help your doctor analyze these tests as well as monitor progression of visual field loss over successive tests.
Ophthalmoscopy
Using an instrument called an ophthalmoscope, your eye doctor can look directly through the pupil at the optic nerve. Its color and appearance can indicate whether or not damage from glaucoma is present and how extensive it is. This technique remains the most important in diagnosing and monitoring glaucoma.
Imaging Technology
A number of new and highly sophisticated image analysis systems are now available to evaluate the optic nerve and retinal nerve fiber layer, the areas of the eye damaged by glaucoma. These devices include scanning laser tomography (e.g. HRT3), laser polarimetry (e.g. GDX), and ocular coherence tomography (e.g. older time-domain OCT or newer spectral-domain OCT). These instruments can help your doctor by giving a quantitative measure of the anatomical structures in the eye. Photographs of the optic nerve can also be useful to follow the progression of damage over time. Large databases have been established to compare an individual's anatomic structures to those of other patients in the same age group. This software and technology are developing rapidly and show great promise. However, they have not yet evolved to replace ophthalmoscopy, where the doctor looks directly at the optic nerve.
A number of new and highly sophisticated image analysis systems are now available to evaluate the optic nerve and retinal nerve fiber layer, the areas of the eye damaged by glaucoma. These devices include scanning laser tomography (e.g. HRT3), laser polarimetry (e.g. GDX), and ocular coherence tomography (e.g. older time-domain OCT or newer spectral-domain OCT). These instruments can help your doctor by giving a quantitative measure of the anatomical structures in the eye. Photographs of the optic nerve can also be useful to follow the progression of damage over time. Large databases have been established to compare an individual's anatomic structures to those of other patients in the same age group. This software and technology are developing rapidly and show great promise. However, they have not yet evolved to replace ophthalmoscopy, where the doctor looks directly at the optic nerve.
Gonioscopy
Your doctor may perform a gonioscopy to closely examine the trabecular meshwork and the angle where fluid drains out of the eye. After dilating and numbing the eye with anesthetic drops, the doctor places a special type of hand-held contact lens, with mirrors inside, on the eye. The mirrors enable the doctor to view the interior of the eye from different directions. In this procedure, the doctor can determine whether the angle is open or narrow. Individuals with narrow angles have an increased risk for a sudeen closure of the angle, which can cause an acute glaucoma attack. Gonioscopy can also determine if anything, such as abnormal blood vessels or excessive pigment, might be blocking the drainage of the aqueous humor out of the eye.
Your doctor may perform a gonioscopy to closely examine the trabecular meshwork and the angle where fluid drains out of the eye. After dilating and numbing the eye with anesthetic drops, the doctor places a special type of hand-held contact lens, with mirrors inside, on the eye. The mirrors enable the doctor to view the interior of the eye from different directions. In this procedure, the doctor can determine whether the angle is open or narrow. Individuals with narrow angles have an increased risk for a sudeen closure of the angle, which can cause an acute glaucoma attack. Gonioscopy can also determine if anything, such as abnormal blood vessels or excessive pigment, might be blocking the drainage of the aqueous humor out of the eye.
The Condition
Glaucoma is a group of eye diseases which in most cases produce increased pressure within the eye. This elevated pressure is caused by a backup of fluid in the eye. Over time, it causes damage to the optic nerve. Through early detection, diagnosis and treatment, you and your doctor can help to preserve your vision.
Think of your eye as a sink, in which the faucet is always running and the drain is always open. The aqueous humor is constantly circulating through the anterior chamber. It is produced by a tiny gland, called the ciliary body, situated behind the iris. It flows between the iris and the lens and, after nourishing the cornea and lens, flows out through a very tiny spongy tissue, only one-fiftieth of an inch wide, called the trabecular meshwork, which serves as the drain of the eye. The trabecular meshwork is situated in the angle where the iris and cornea meet. When this drain becomes clogged, aqueous can not leave the eye as fast as it is produced, causing the fluid to back up. But since the eye is a closed compartment, your `sink´ doesn´t overflow; instead the backed up fluid causes increased pressure to build up within the eye. We call this open (wide) angle glaucoma.
To understand how this increased pressure affects the eye, think of your eye as a balloon. When too much air is blown into the balloon, the pressure builds, causing it to pop. But the eye is too strong to pop. Instead, it gives at the weakest point, which is the site in the sclera at which the optic nerve leaves the eye.
The optic nerve is part of the central nervous system and carries visual information from the eye to the brain. This cranial nerve is made up of over one million nerve axons, which are nerve fiber extensions of the retinal ganglion cells. When the eye pressure is increased and/or other inciting factors exist, the optic nerve becomes damaged and the retinal ganglion cells undergo a slow process of cell death termed "apoptosis." The death of the retinal cells and degeneration of the nerve fibers results in permanent vision loss. Early diagnosis and treatment of glaucoma can help prevent blindness.
Think of your eye as a sink, in which the faucet is always running and the drain is always open. The aqueous humor is constantly circulating through the anterior chamber. It is produced by a tiny gland, called the ciliary body, situated behind the iris. It flows between the iris and the lens and, after nourishing the cornea and lens, flows out through a very tiny spongy tissue, only one-fiftieth of an inch wide, called the trabecular meshwork, which serves as the drain of the eye. The trabecular meshwork is situated in the angle where the iris and cornea meet. When this drain becomes clogged, aqueous can not leave the eye as fast as it is produced, causing the fluid to back up. But since the eye is a closed compartment, your `sink´ doesn´t overflow; instead the backed up fluid causes increased pressure to build up within the eye. We call this open (wide) angle glaucoma.
To understand how this increased pressure affects the eye, think of your eye as a balloon. When too much air is blown into the balloon, the pressure builds, causing it to pop. But the eye is too strong to pop. Instead, it gives at the weakest point, which is the site in the sclera at which the optic nerve leaves the eye.
The optic nerve is part of the central nervous system and carries visual information from the eye to the brain. This cranial nerve is made up of over one million nerve axons, which are nerve fiber extensions of the retinal ganglion cells. When the eye pressure is increased and/or other inciting factors exist, the optic nerve becomes damaged and the retinal ganglion cells undergo a slow process of cell death termed "apoptosis." The death of the retinal cells and degeneration of the nerve fibers results in permanent vision loss. Early diagnosis and treatment of glaucoma can help prevent blindness.
Types of Glaucoma
Primary close angle glaucoma
Approximately one percent of all Americans have this form of glaucoma, making it the most common form of glaucoma in our country. It occurs mainly in the over 50 age group.
There are no symptoms associated with POAG. The pressure in the eye slowly rises and the cornea adapts without swelling. If the cornea were to swell, which is usually a signal that something is wrong, symptoms would be present. But as this is not the case, this disease often goes undetected. It is painless, and the patient often does not realize that he or she is slowly losing vision until the later stages of the disease. However, by the time the vision is impaired, the damage is irreversible.
In POAG, there is no visible abnormality of the trabecular meshwork. It is believed that something is wrong with the ability of the cells in the trabecular meshwork to carry out their normal function, or there may be fewer cells present, as a natural result of getting older. Some believe it is due to a structural defect of the eye´s drainage system. Others believe it is caused by an enzymatic problem. These theories, as well as others, are currently being studied and tested at numerous research centers across the country.
Glaucoma is really about the problems which occur as a result of increased IOP. The average IOP in a normal population is 14-16 millimeters of mercury (mmHg). In a normal population pressures up to 20 mmHg may be within normal range. A pressure of 22 is considered to be suspicious and possibly abnormal. However, not all patients with elevated IOP develop glaucoma-related eye damage. What causes one person to develop damage while another does not is a topic of active research.
As we mentioned earlier, this increased pressure can ultimately destroy the optic nerve cells. Once a sufficient number of nerve cells are destroyed, blind spots begin to form in the field of vision. These blind spots usually develop first in the peripheral field of vision, the outer sides of the field of vision. In the later stages, the central vision, which we experience as `seeing,´ is affected. Once visual loss occurs, it is irreversible because once the nerve cells are dead, nothing can restore them at the present time. Later on, we will talk about the many ways your eye doctor can detect glaucoma in its earliest stages -- before any visual damage occurs.
POAG is a chronic disease. It may be hereditary. There is no cure for it at present, but the disease can be slowed or arrested by treatment. Since there are no symptoms, many patients find it difficult to understand why lifelong treatment with expensive drugs is necessary, especially when these drugs are often bothersome to take and have a variety of side effects.
Taking medications regularly, as prescribed, is crucial to preventing vision-threatening damage. That is why it is important for you to discuss these side effects with your doctor. The two of you need to act as a `team´ in the battle against glaucoma. Later on, we will discuss the medications commonly prescribed and their side effects
There are no symptoms associated with POAG. The pressure in the eye slowly rises and the cornea adapts without swelling. If the cornea were to swell, which is usually a signal that something is wrong, symptoms would be present. But as this is not the case, this disease often goes undetected. It is painless, and the patient often does not realize that he or she is slowly losing vision until the later stages of the disease. However, by the time the vision is impaired, the damage is irreversible.
In POAG, there is no visible abnormality of the trabecular meshwork. It is believed that something is wrong with the ability of the cells in the trabecular meshwork to carry out their normal function, or there may be fewer cells present, as a natural result of getting older. Some believe it is due to a structural defect of the eye´s drainage system. Others believe it is caused by an enzymatic problem. These theories, as well as others, are currently being studied and tested at numerous research centers across the country.
Glaucoma is really about the problems which occur as a result of increased IOP. The average IOP in a normal population is 14-16 millimeters of mercury (mmHg). In a normal population pressures up to 20 mmHg may be within normal range. A pressure of 22 is considered to be suspicious and possibly abnormal. However, not all patients with elevated IOP develop glaucoma-related eye damage. What causes one person to develop damage while another does not is a topic of active research.
As we mentioned earlier, this increased pressure can ultimately destroy the optic nerve cells. Once a sufficient number of nerve cells are destroyed, blind spots begin to form in the field of vision. These blind spots usually develop first in the peripheral field of vision, the outer sides of the field of vision. In the later stages, the central vision, which we experience as `seeing,´ is affected. Once visual loss occurs, it is irreversible because once the nerve cells are dead, nothing can restore them at the present time. Later on, we will talk about the many ways your eye doctor can detect glaucoma in its earliest stages -- before any visual damage occurs.
POAG is a chronic disease. It may be hereditary. There is no cure for it at present, but the disease can be slowed or arrested by treatment. Since there are no symptoms, many patients find it difficult to understand why lifelong treatment with expensive drugs is necessary, especially when these drugs are often bothersome to take and have a variety of side effects.
Taking medications regularly, as prescribed, is crucial to preventing vision-threatening damage. That is why it is important for you to discuss these side effects with your doctor. The two of you need to act as a `team´ in the battle against glaucoma. Later on, we will discuss the medications commonly prescribed and their side effects
Low-tension glaucoma
Normal-tension glaucoma, also known as low-tension glaucoma, is characterized by progressive optic nerve damage and visual field loss with a statistically normal intraocular pressure. This form of glaucoma, which is being increasingly recognized, may account for as many as one-third of the cases of open-angle glaucoma in the United States.Normal-tension glaucoma is thought to be related, at least in part, to poor blood flow to the optic nerve, which leads to death of the cells which carry impulses from the retina to the brain. In addition, these eyes appear to be susceptible to pressure-related damage even in the high normal range, and therefore a pressure lower than normal is often necessary to prevent further visual loss.
Research in the field of optic nerve blood flow and its role in glaucoma is a source of much excitement at the present time and, hopefully, will lead to new methods of treating this disorder. Since the best therapy for normal-tension glaucoma is largely unknown, much attention is being given to a study known as the International Collaborative Low Tension Glaucoma Protocol.
Close angle Glaucoma
There is a tendency for this disease to be inherited, and often several members of a family will be afflicted. It is most common in people of Asian descent and people who are far-sighted.
In people with a tendency to angle-closure glaucoma, the anterior chamber is smaller than average. As mentioned earlier, the trabecular meshwork is situated in the angle formed where the cornea and the iris meet. In most people, this angle is about 45 degrees. The narrower the angle, the closer the iris is to the trabecular meshwork. As we age, the lens routinely grows larger. The ability of aqueous humor to pass between the iris and lens on its way to the anterior chamber becomes decreased, causing fluid pressure to build up behind the iris, further narrowing the angle. If the pressure becomes sufficiently high, the iris is forced against the trabecular meshwork, blocking drainage, similar to putting a stopper over the drain of a sink. When this space becomes completely blocked, an angle-closure glaucoma attack (acute glaucoma) results.
In people with a tendency to angle-closure glaucoma, the anterior chamber is smaller than average. As mentioned earlier, the trabecular meshwork is situated in the angle formed where the cornea and the iris meet. In most people, this angle is about 45 degrees. The narrower the angle, the closer the iris is to the trabecular meshwork. As we age, the lens routinely grows larger. The ability of aqueous humor to pass between the iris and lens on its way to the anterior chamber becomes decreased, causing fluid pressure to build up behind the iris, further narrowing the angle. If the pressure becomes sufficiently high, the iris is forced against the trabecular meshwork, blocking drainage, similar to putting a stopper over the drain of a sink. When this space becomes completely blocked, an angle-closure glaucoma attack (acute glaucoma) results.
Acute Glaucoma
Unlike POAG (Primary Open-Angle Glaucoma), where the IOP increases slowly, in acute angle-closure, it increases suddenly. This sudden rise in pressure can occur within a matter of hours and become very painful. If the pressure rises high enough, the pain may become so intense that it can cause nausea and vomiting.
The eye becomes red, the cornea swells and clouds, and the patient may see haloes around lights and experience blurred vision.
An acute attack is an emergency condition. If treatment is delayed, eyesight can be permanently destroyed. Scarring of the trabecular meshwork may occur and result in chronic glaucoma, which is much more difficult to control. Cataracts may also develop. Damage to the optic nerve may occur quickly and cause permanently impaired vision.
Many of these sudden attacks occur in darkened rooms, such as movie theaters. If you recall, darkened environments cause the pupil to dilate, or increase in size. When this happens, there is maximum contact between the eye´s lens and the iris. This further narrows the angle and may trigger an attack. But the pupil also dilates when one is excited or anxious. Consequently, many acute glaucoma attacks occur during periods of stress. A variety of drugs can also cause dilation of the pupil and lead to an attack of glaucoma. These include anti-depressants, cold medications, antihistamines, and some medications to treat nausea.
Acute glaucoma attacks are not always full blown. Sometimes a patient may have a series of minor attacks. A slight blurring of vision and haloes (rainbow-colored rings around lights) may be experienced, but without pain or redness. These attacks may end when the patient enters a well lit room or goes to sleep -- two situations which naturally cause the pupil to constrict, thereby allowing the iris to pull away from the drain.
An acute attack may be stopped with a combination of drops which constrict the pupil, and drugs that help reduce the eye´s fluid production. As soon as the IOP has dropped to a safe level, your ophthalmologist will perform a laser iridotomy. A laser iridotomy is an outpatient procedure in which a laser beam is used to make a small opening in the iris. This allows the fluid to flow more freely. Drops will be used to anesthetize your eye and there is no pain involved. The entire procedure should take less than thirty minutes. Laser surgery may be performed prophylactically on the other eye, as well. Since it is common for both eyes to suffer from narrowed angles, operating on the unaffected eye is done as a preventive measure.
Routine examinations using a technique called gonioscopy can predict one´s chances of having an acute attack. A special lens which contains a mirror is placed lightly on the front of the eye and the width of the angle examined visually. Patients with narrow angles can be warned of early symptoms, so that they can seek immediate treatment. In some cases, laser treatment is recommended as a preventive measure.
Not all angle-closure glaucoma sufferers will experience an acute attack. Instead, some may develop what is called chronic angle-closure glaucoma. In this case, the iris gradually closes over the drain, causing no overt symptoms. When this occurs, scars slowly form between the iris and the drain and the IOP will not rise until there is a significant amount of scar tissue formed -- enough to cover the drainage area. If the patient is treated with medication, such as pilocarpine, an acute attack may be prevented, but the chronic form of the disease may still develop.
The eye becomes red, the cornea swells and clouds, and the patient may see haloes around lights and experience blurred vision.
An acute attack is an emergency condition. If treatment is delayed, eyesight can be permanently destroyed. Scarring of the trabecular meshwork may occur and result in chronic glaucoma, which is much more difficult to control. Cataracts may also develop. Damage to the optic nerve may occur quickly and cause permanently impaired vision.
Many of these sudden attacks occur in darkened rooms, such as movie theaters. If you recall, darkened environments cause the pupil to dilate, or increase in size. When this happens, there is maximum contact between the eye´s lens and the iris. This further narrows the angle and may trigger an attack. But the pupil also dilates when one is excited or anxious. Consequently, many acute glaucoma attacks occur during periods of stress. A variety of drugs can also cause dilation of the pupil and lead to an attack of glaucoma. These include anti-depressants, cold medications, antihistamines, and some medications to treat nausea.
Acute glaucoma attacks are not always full blown. Sometimes a patient may have a series of minor attacks. A slight blurring of vision and haloes (rainbow-colored rings around lights) may be experienced, but without pain or redness. These attacks may end when the patient enters a well lit room or goes to sleep -- two situations which naturally cause the pupil to constrict, thereby allowing the iris to pull away from the drain.
An acute attack may be stopped with a combination of drops which constrict the pupil, and drugs that help reduce the eye´s fluid production. As soon as the IOP has dropped to a safe level, your ophthalmologist will perform a laser iridotomy. A laser iridotomy is an outpatient procedure in which a laser beam is used to make a small opening in the iris. This allows the fluid to flow more freely. Drops will be used to anesthetize your eye and there is no pain involved. The entire procedure should take less than thirty minutes. Laser surgery may be performed prophylactically on the other eye, as well. Since it is common for both eyes to suffer from narrowed angles, operating on the unaffected eye is done as a preventive measure.
Routine examinations using a technique called gonioscopy can predict one´s chances of having an acute attack. A special lens which contains a mirror is placed lightly on the front of the eye and the width of the angle examined visually. Patients with narrow angles can be warned of early symptoms, so that they can seek immediate treatment. In some cases, laser treatment is recommended as a preventive measure.
Not all angle-closure glaucoma sufferers will experience an acute attack. Instead, some may develop what is called chronic angle-closure glaucoma. In this case, the iris gradually closes over the drain, causing no overt symptoms. When this occurs, scars slowly form between the iris and the drain and the IOP will not rise until there is a significant amount of scar tissue formed -- enough to cover the drainage area. If the patient is treated with medication, such as pilocarpine, an acute attack may be prevented, but the chronic form of the disease may still develop.
Pigmentary glaucoma
Pigmentary glaucoma is a type of inherited open-angle glaucoma which develops more frequently in men than in women. It most often begins in the twenties and thirties, which makes it particularly dangerous to a lifetime of normal vision. Nearsighted patients are more typically afflicted. The anatomy of the eyes of these patients appears to play a key role in the development of this type of glaucoma. Let us examine why.Myopic (nearsighted) eyes have a concave-shaped iris which creates an unusually wide angle. This causes the pigment layer of the eye to rub on the lens. This rubbing action causes the iris pigment to shed into the aqueous humor and onto neighboring structures, such as the trabecular meshwork. Pigment may plug the pores of the trabecular meshwork, causing it to clog, and thereby increasing the IOP.
Miotic therapy is the treatment of choice, but these drugs in drop form can cause disabling visual blurring in younger patients.
Fortunately, a slow-release form is available. Laser iridotomy is presently being investigated in the treatment of this disorder.
Exfoliation syndrome
This common cause of glaucoma is found everywhere in the world, but is most common among people of European descent. In about 10% of the population over age 50, a whitish material, which looks on slit-lamp examination somewhat like tiny flakes of dandruff, builds up on the lens of the eye. This exfoliation material is rubbed off the lens by movement of the iris and at the same time, pigment is rubbed off the iris. Both pigment and exfoliation material clog the trabecular meshwork, leading to IOP elevation, sometimes to very high levels.Exfoliation syndrome can lead to both open-angle glaucoma and angle-closure glaucoma, often producing both kinds of glaucoma in the same individual. Not all persons with exfoliation syndrome develop glaucoma. However, if you have exfoliation syndrome, your chances of developing glaucoma are about six times as high as if you don´t. It often appears in one eye long before the other, for unknown reasons. If you have glaucoma in one eye only, this is the most likely cause. It can be detected before the glaucoma develops, so that you can be more carefully observed and minimize your chances of vision loss.
Trauma Related Glaucoma
A blow to the eye, chemical burn, or penetrating injury may all lead to the development of glaucoma, either acute or chronic. This can be due to a mechanical disruption or physical change within the eye´s drainage system. It is therefore crucial for anyone who has suffered eye trauma to have check-ups at regular intervals
Childhood Glaucoma
Childhood glaucoma is an unusual eye disease and significant cause of childhood blindness. It is caused by disease related abnormal increase in intraocular pressure. The multiple potential causes fall into one of two categories and may be primary or secondary to some other disease process. Primary congenital glaucoma results from abnormal development of the ocular drainage system. It occurs in about 1 out of 10,000 births in the United States and is the most common form of glaucoma in infants. Secondary glaucomas result from disorders of the body or eye and may or may not be genetic. Both types may be associated with other medical diseases.Ten percent of primary congenital glaucomas are present at birth, and 80 percent are diagnosed during the first year of life. The pediatrician or family first notice eye signs of glaucoma including clouding and/or enlargement of the cornea. The elevated intraocular pressure (IOP) can cause the eyeball itself to enlarge and injury to the cornea. Important early symptoms of glaucoma in infants and children are poor vision, light sensitivity, tearing, and blinking.
Pediatric glaucoma is treated differently than adult glaucoma. Most patients require surgery and this is typically performed early. The aim of pediatric glaucoma surgery is to reduce IOP either by increasing the outflow of fluid from the eye or decrease the production of fluid within the eye. One operation for pediatric glaucoma is goniotomy. Its rate of success is associated with the age of the child at the time of diagnosis, the type and severity of the glaucoma, and the surgery technique. Other surgical options are trabeculectomy and glaucoma drainage tubes.
Approximately 80-90 percent of babies who receive prompt surgical treatment, long-term care, and monitoring of their visual development will do well, and may have normal or nearly normal vision for their lifetime. Sadly, primary congenital glaucoma results in blindness in 2 to 15 percent of childhood patients. When childhood glaucoma is not recognized and treated promptly more permanent visual loss will result.
The Treatment
Glaucoma can be treated with eye drops, pills, laser surgery, traditional surgery or a combination of these methods. The goal of any treatment is to prevent loss of vision, as vision loss from glaucoma is irreversible. The good news is that glaucoma can be managed if detected early, and that with medical and/or surgical treatment, most people with glaucoma will not lose their sight.
Taking medications regularly, as prescribed, is crucial to preventing vision-threatening damage. That is why it is important for you to discuss side effects with your doctor. While every drug has some potential side effects, it is important to note that many patients experience no side effects at all. You and your doctor need to work as a team in the battle against glaucoma. Your doctor has many options. They include:
Eye Drops
It is important to take your medications regularly and exactly as prescribed if you are to control your eye pressure. Since eye drops are absorbed into the bloodstream, tell your doctor about all medications you are currently taking. Ask your doctor and/or pharmacist if the medications you are taking together are safe. Some drugs can be dangerous when mixed with other medications. To minimize absorption into the bloodstream and maximize the amount of drug absorbed in the eye, close your eye for one to two minutes after administering the drops and press your index finger lightly against the inferior nasal corner of your eyelid to close the tear duct which drains into the nose. While almost all eye drops may cause an uncomfortable burning or stinging sensation at first, the discomfort should last for only a few seconds.
It is important to take your medications regularly and exactly as prescribed if you are to control your eye pressure. Since eye drops are absorbed into the bloodstream, tell your doctor about all medications you are currently taking. Ask your doctor and/or pharmacist if the medications you are taking together are safe. Some drugs can be dangerous when mixed with other medications. To minimize absorption into the bloodstream and maximize the amount of drug absorbed in the eye, close your eye for one to two minutes after administering the drops and press your index finger lightly against the inferior nasal corner of your eyelid to close the tear duct which drains into the nose. While almost all eye drops may cause an uncomfortable burning or stinging sensation at first, the discomfort should last for only a few seconds.
Pills
Sometimes, when eye drops don't sufficiently control IOP, pills may be prescribed in addition to drops. These pills, which have more systemic side effects than drops, also serve to turn down the eye's faucet and lessen the production of fluid. These medications are usually taken from two to four times daily. It is important to share this information with all your other doctors so they can prescribe medications for you which will not cause potentially dangerous interactions.
Sometimes, when eye drops don't sufficiently control IOP, pills may be prescribed in addition to drops. These pills, which have more systemic side effects than drops, also serve to turn down the eye's faucet and lessen the production of fluid. These medications are usually taken from two to four times daily. It is important to share this information with all your other doctors so they can prescribe medications for you which will not cause potentially dangerous interactions.
Surgical Procedures
When medications do not achieve the desired results, or have intolerable side effects, your ophthalmologist may suggest surgery.
When medications do not achieve the desired results, or have intolerable side effects, your ophthalmologist may suggest surgery.
Laser Surgery
Laser surgery has become increasingly popular as an intermediate step between drugs and traditional surgery though the long-term success rates are variable. The most common type performed for open-angle glaucoma is called trabeculoplasty. This procedure takes between 10 and 15 minutes, is painless, and can be performed in either a doctor's office or an outpatient facility. The laser beam (a high energy light beam) is focused upon the eye's drain. Contrary to what many people think, the laser does not bum a hole through the eye. Instead, the eye's drainage system is changed in very subtle ways so that aqueous fluid is able to pass more easily out of the drain, thus lowering IOP.
You may go home and resume your normal activities following surgery. Your doctor will likely check your IOP one to two hours following laser surgery. After this procedure, many patients respond well enough to be able to avoid or delay surgery. While it may take a few weeks to see the full pressure-lowering effect of this procedure, during which time you may have to continue taking your medications, many patients are eventually able to discontinue some of their medications. This, however, is not true in all cases. Your doctor is the best judge of determining whether or not you will still need medication. Complications from laser are minimal, which is why this procedure has become increasingly popular and some centers are recommending the use of laser before drops in some patients.
Argon Laser Trabeculoplasty (ALT) -- for open-angle glaucoma
The laser treats the trabecular meshwork of the eye, increasing the drainage outflow, thereby lowering the IOP. In many cases, medication will still be needed. Usually, half the trabecular meshwork is treated first. If necessary, the other half can be treated as a separate procedure. This method decreases the risk of increased pressure following surgery. Argon laser trabeculoplasty has successfully lowered eye pressure in up to 75 percent of patients treated. This type of laser can be performed only two to three times in each eye over a lifetime.
Selective Laser Trabeculoplasty (SLT) -- for open-angle glaucoma
SLT is a newer laser that uses very low levels of energy. It is termed "selective" since it leaves portions of the trabecular meshwork intact. For this reason, it is believed that SLT, unlike other types of laser surgery, may be safely repeated. Some authors have reported that a second repeat application of SLT or SLT after prior ALT is effective at lowering IOP.
Laser Peripheral Iridotomy (LPI) -- for angle-closure glaucoma
This procedure is used to make an opening through the iris, allowing aqueous fluid to flow from behind the iris directly to the anterior chamber of the eye. This allows the fluid to bypass its normal route. LPI is the preferred method for managing a wide variety of angle-closure glaucomas that have some degree of pupillary blockage. This laser is most often used to treat an anatomically narrow angle and prevent angle-closure glaucoma attacks.
Cycloablation
Two laser procedures for open-angle glaucoma involve reducing the amount of aqueous humor in the eye by destroying part of the ciliary body, which produces the fluid. These treatments are usually reserved for use in eyes that either have elevated IOP after having failed other more traditional treatments, including filtering surgery, or those in which filtering surgery is not possible or advisable due to the shape or other features of the eye. Transscleral cyclophotocoagulation uses a laser to direct energy through the outer sclera of the eye to reach and destroy portions of the ciliary processes, without causing damage to the overlying tissues. With endoscopic cyclophotocoagulation (ECP), the instrument is placed inside the eye through a surgical incision, so that the laser energy is applied directly to the ciliary body tissue.
Traditional Surgery
Trabeculectomy
When medications and laser therapies do not adequately lower eye pressure, doctors may recommend conventional surgery. The most common of these operations is called a trabeculectomy, which is used in both open-angle and closed-angle glaucomas. In this procedure, the surgeon creates a passage in the sclera (the white part of the eye) for draining excess eye fluid. A flap is created that allows fluid to escape, but which does not deflate the eyeball. A small bubble of fluid called a "bleb" often forms over the opening on the surface of the eye, which is a sign that fluid is draining out into the space between the sclera and conjunctiva. Occasionally, the surgically created drainage hole begins to close and the IOP rises again. This happens because the body tries to heal the new opening, as if it was an injury. Many surgeons perform trabeculectomy with an anti-fibrotic agent that is placed on the eye during surgery and reduces such scarring during the healing period. The most common anti-fibrotic agent is Mitomycin-C. Another is 5-Fluorouracil, or 5-FU.
About 50 percent of patients no longer require glaucoma medications after surgery for a significant length of time. Thirty-five to 40 percent of those who still need medication have better control of their IOP. A trabeculectomy is usually an outpatient procedure. The number of post-operative visits to the doctor varies, and some activities, such as driving, reading, bending and heavy lifting must be limited for two to four weeks after surgery.
Drainage Implant Surgery
Several different devices have been developed to aid the drainage of aqueous humor out of the anterior chamber and lower IOP. All of these drainage devices share a similar design which consists of a small silicone tube that extends into the anterior chamber of the eye. The tube is connected to one or more plates, which are sutured to the surface of the eye, usually not visible. Fluid is collected on the plate and then absorbed by the tissues in the eye. This type of surgery is thought to lower IOP less than trabeculectomy but is preferred in patients whose IOP cannot be controlled with traditional surgery or who have previous scarring.
Nonpenetrating Surgery
Newer nonpenetrating glaucoma surgery, which does not enter the anterior chamber of the eye, shows great promise in minimizing postoperative complications and lowering the risk for infection. However, such surgery often requires a greater surgical acument and generally does not lower IOP as much as trabeculectomy. Furthermore, long term studies are needed to assess these procedures and to determine their role in the clinical management of glaucoma patients.
Some Promising Surgical Alternatives
The ExPress mini glaucoma shunt is a stainless steel device that is inserted into the anterior chamber of the eye and placed under a scleral flap. It lowers IOP by diverting aqueous humor from the anterior chamber. The ExPress offers the glaucoma surgeon an alternative to either repeating a trabeculectomy or placing a more extensive silicone tube shunt in those patients whose IOP is higher than the optic nerve can tolerate.
The Trabectome is a new probe-like device that is inserted into the anterior chamber through the cornea. The procedure uses a small probe that opens the eye's drainage system through a tiny incision and delivers thermal energy to the trabecular meshwork, reducing resistance to outflow of aqueous humor and, as a result, lowering IOP.
Canaloplasty, a recent advancement in non-penetrating surgery, is designed to improve the aqueous circulation through the trabecular outflow process, thereby reducing IOP. Unlike traditional trabeculectomy, which creates a small hole in the eye to allow fluid to drain out, canaloplasty has been compared to an ocular version of angioplasty, in which the physician uses an extremely fine catheter to clear the drainage canal.
glasses online 241 glasses including lenses free post
Michael Caine Legendary Icon The Next King of England

Mr Micheal Caine simply one of the icon’s of our time and someone who’s films will be timeless. Get the iconic glasses with a twist .Designer glasses online. 2 for 1 on all glasses lenses and coatings free delivery and prices from £50

Micheal Caine



 super cool micheal caine even when just reading the paperstone cold coolmicheal caine relaxing with the ladiesMicheal Caine "Alfie"
super cool micheal caine even when just reading the paperstone cold coolmicheal caine relaxing with the ladiesMicheal Caine "Alfie"




Saturday 30 July 2011
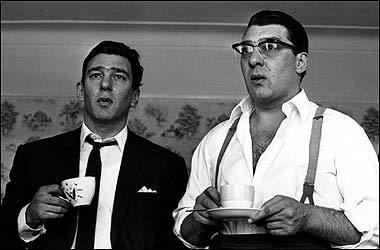
Kray Twins

love them or hate them the krays have an icon status as Britains only true Gangsters of any note. They had a style all of their own get the look from suitsto glasses to shoes to hankerchiefs to shirts and ties. Get designer glasses online ,2 4 1 on glasses lenses and treatments. free postage to anywhere
Friday 29 July 2011
Graham Coxon, Blur

Graham Coxon one of the nerdiest geniuses of all time but ultimately sumblimely cool as it has been proved get the look with a twist of lime.Designer glasses online 2for1 on all glasses lenses and treatments and free delivery!!!!!!.
Thursday 28 July 2011
James Dean King of Super Cool
















James Dean king of super cool
will anyone ever look this good in glasses again
get glasses online from £50 buy one get one free
designer glasses online From £99 buy one get one free
Free postage to anywhere
http://www.freshoptical.co.uk/http://www.freshoptical.co.uk/http://www.freshoptical.co.uk/http://www.freshoptical.co.uk/james deanjames deanjames deanhttp://www.freshoptical.co.uk/james deanjames deanjames deanjames deanjames deanjames deanjames deanJames Dean
James Dean King of Super Cool
















James Dean king of super cool
will anyone ever look this good in glasses again
get glasses online from £50 buy one get one free
designer glasses online From £99 buy one get one free
Free postage to anywhere
http://www.freshoptical.co.uk/http://www.freshoptical.co.uk/http://www.freshoptical.co.uk/http://www.freshoptical.co.uk/james deanjames deanjames deanhttp://www.freshoptical.co.uk/james deanjames deanjames deanjames deanjames deanjames deanjames deanJames Dean
Subscribe to:
Posts (Atom)